Early in the Omicron wave in South Africa some local doctors were commenting that they were seeing many “mild” cases of Omicron, quite different from what they had seen with Delta in the previous wave in the country.
Soon there were two competing takes on Omicron in the public discourse, one that concludes that Omicron is more like a bad cold and another that the true virulence of Omicron, even if it was somewhat lower, would matter less than the larger number of cases from its rapid spread. “A small percentage of a very large number can also be a large number,” is how many of the experts cautioned us.
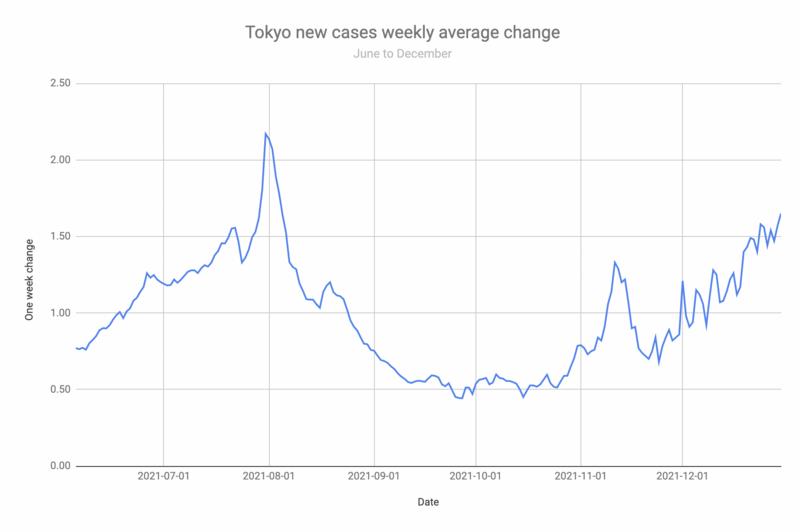
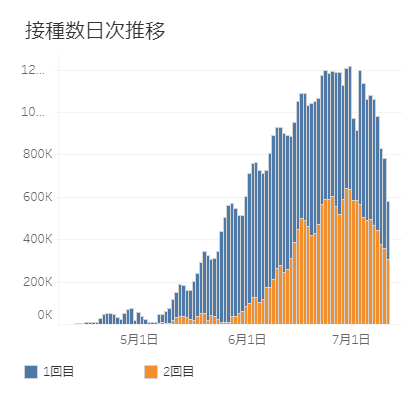
The picture was further clouded by the fact that Omicron was spreading in parallel with Delta: Many of the countries that were seeing Omicron waves were already in the midst of a Delta wave connected to the onset of winter in the northern hemisphere. For example, Japan had cases growing about 20 percent week on week for several weeks before it saw significant numbers of confirmed Omicron cases. Many of the deaths seen while Omicron cases were already growing rapidly were still Delta cases.
Death numbers always lag a few weeks behind case numbers. For example, in Tokyo the average gap between Covid diagnosis and death is about 15 days. Then it takes another 16 days on average for the death to be reported in the evening news. This means, the death count reported in the media was from people who on average died 16 days ago after having a positive PCR test 31 days ago. The positive result of the PCR test would have been included in the daily count on average about 2-3 days after the test was taken.
There is some evidence that Omicron is less virulent than Delta. A study on hamsters showed that the variant seems less capable of infecting lung cells and seems to be more focussed on the nose, throat and windpipe, which may also contribute to its easier spread. It’s not clear how these animal study results translate to humans. In December, different numbers were reported for how much less virulent Omicron was overall or specifically for unvaccinated people, with risk reductions mentioned anywhere from 15 to 70 percent.
In any case, milder than Delta does not mean mild: Delta was worse than Alpha which was worse than the D614G strain that devastated Italy and New York city in March 2020, which was worse than the original Wuhan strain. Omicron may still be as bad as one of its pre-Delta ancestors, which were deadly enough.
Finally, we have some numbers coming in.
During the Delta wave the UK 7-day trailing count of deaths had reached a peak of around 1,200 in early November 2021, when almost 100% of cases were still Delta. On January 14, 2022, when most UK cases were Omicron, this had increased to about 1,800 deaths in the last 7 days, about 50 percent more deaths per week than at the peak of Delta.
The picture is similar in Canada, where 7-day deaths peaked at 344 in October with Delta. On January 15, 2022 the same metric reached 606, almost twice as deadly, with Omicron.
While the Case Fatality Rate (CFR), which is defined as the number of deaths divided by confirmed cases, has declined with Omicron relative to Delta, this is primarily because of the extraordinarily rapid growth of cases, which grew faster than deaths climbed. The CFR went down even as deaths increase. Thus Omicron can appear to be milder and not so mild after all, as it ends up killing more people per week than Delta did. If cases go up 5-fold but deaths “only” double, the CFR will fall by 60 percent.
The only saving grace may be that Omicron will most likely burn through the infectable population more quickly than Delta ever did. Cases have peaked in South Africa, the UK and most of the US. By February they will probably also peak in Japan (before I and most others can get a booster here).
Wear a good mask, if you meet people do it outdoors, ventilate, get vaccinated and get a booster if you can.
Links: